- Research
- Open Access
Medical implications of technical accuracy in genome sequencing
- Rachel L. Goldfeder†1, 3,
- James R. Priest†3, 5,
- Justin M. Zook†2,
- Megan E. Grove1, 3,
- Daryl Waggott1, 3,
- Matthew T. Wheeler1, 3,
- Marc Salit†2 and
- Euan A. Ashley†1, 3, 4Email author
- Received: 21 August 2015
- Accepted: 21 January 2016
- Published: 2 March 2016
Abstract
Background
As whole exome sequencing (WES) and whole genome sequencing (WGS) transition from research tools to clinical diagnostic tests, it is increasingly critical for sequencing methods and analysis pipelines to be technically accurate. The Genome in a Bottle Consortium has recently published a set of benchmark SNV, indel, and homozygous reference genotypes for the pilot whole genome NIST Reference Material based on the NA12878 genome.
Methods
We examine the relationship between human genome complexity and genes/variants reported to be associated with human disease. Specifically, we map regions of medical relevance to benchmark regions of high or low confidence. We use benchmark data to assess the sensitivity and positive predictive value of two representative sequencing pipelines for specific classes of variation.
Results
We observe that the accuracy of a variant call depends on the genomic region, variant type, and read depth, and varies by analytical pipeline. We find that most false negative WGS calls result from filtering while most false negative WES variants relate to poor coverage. We find that only 74.6 % of the exonic bases in ClinVar and OMIM genes and 82.1 % of the exonic bases in ACMG-reportable genes are found in high-confidence regions. Only 990 genes in the genome are found entirely within high-confidence regions while 593 of 3,300 ClinVar/OMIM genes have less than 50 % of their total exonic base pairs in high-confidence regions. We find greater than 77 % of the pathogenic or likely pathogenic SNVs currently in ClinVar fall within high-confidence regions. We identify sites that are prone to sequencing errors, including thousands present in publicly available variant databases. Finally, we examine the clinical impact of mandatory reporting of secondary findings, highlighting a false positive variant found in BRCA2.
Conclusions
Together, these data illustrate the importance of appropriate use and continued improvement of technical benchmarks to ensure accurate and judicious interpretation of next-generation DNA sequencing results in the clinical setting.
Keywords
- Whole Genome Sequencing
- Whole Exome Sequencing
- OMIM Gene
- Base Quality Score Recalibration
- False Positive Variant
Background
As whole exome sequencing (WES) and whole genome sequencing (WGS) transition from research tools to clinical diagnostic tests, it is increasingly critical for sequencing methods and analysis pipelines to be technically accurate. To interpret appropriately the results of any clinical test, the informed clinician should have a working knowledge of the accuracy and diagnostic characteristics of the test. Initial evaluations suggest that SNV and INDEL genotype calls can vary based on exome capture kit, sequencing platform, and the aligner and variant caller [1–9]. An absence of technical benchmark data and evaluation methods prompted the National Institute of Standards and Technology (NIST) to convene the Genome in a Bottle (GIAB) Consortium to develop infrastructure to address this problem. The consortium is developing and disseminating Reference Materials, Reference Data, and Reference Methods for human genome sequencing.
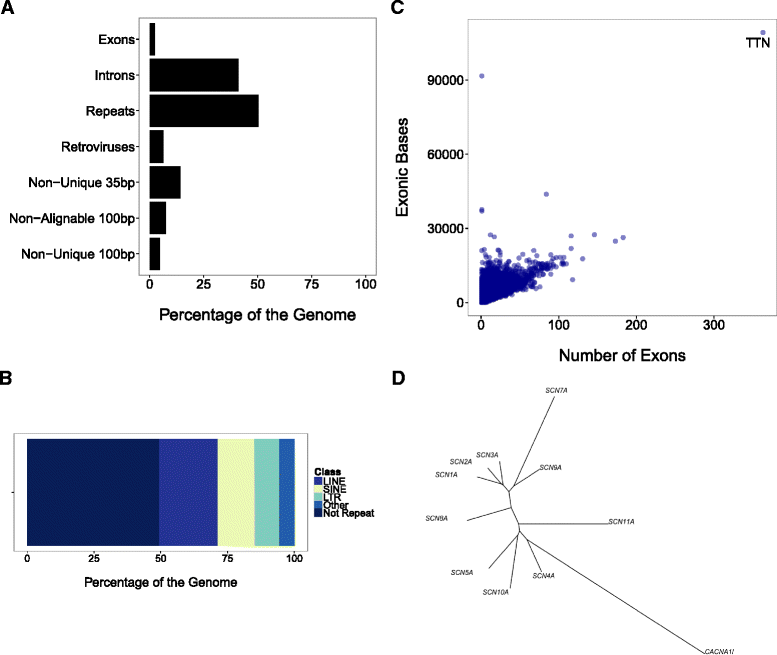
Complexity of the Genome. a The genome consists of several (overlapping) regions. Eighty-six percent of 35 bp sequences and 95 % of 100 bp sequences are unique to one location in the reference genome. b A total of 50.6 % of the non-N reference genome falls into a repeat (data from RepeatMasker). c There is great variation in exon count and number of exonic bases per gene (data from RefSeq). d An unrooted phylogenetic tree derived from multiple alignment of cDNA sequences of 10 voltage-gated sodium channel genes within the human genome illustrates the complexity evolutionary relationship of paralogous sequences which complicates the process of short-read alignment in next-generation sequencing. A related voltage gated calcium channel CACNA1L is included as an outgroup
Over the last several years many groups have demonstrated the clinical utility of genome sequencing [14–17], developing tools for clinical interpretation of individuals [18], families [19], and for rapid genetic diagnosis [20–24]. Themes throughout this work include low concordance across platforms for insertion-deletion variants, and moderate concordance between interpreters of genomic variants [1, 5, 25].
In this analysis, we characterize the GIAB [26] high-confidence regions, benchmark WGS and WES example variant calls in relation to publicly available high-confidence consensus SNV, indel, and homozygous reference genotypes for NA12878, and evaluate the clinical impact of genomic sites with systematic errors from one or more sequencing platforms. We use the WGS and WES benchmark to investigate the causes of extra and missing variants in two call sets (putative false positive and false negative variants, respectively). We focus on potentially functionally significant variants. Finally, we compare performance across the whole genome to performance for different types of potentially functional variants in genes that have different levels of evidence for disease association and clinical actionability.
Methods
Reference genome, sequencing platforms, and variant calling
We recently published a set of high-confidence SNV, indel, and homozygous reference genotypes for the pilot whole genome NIST Reference Material 8398 [26]. Briefly these genotypes were generated by integrating 14 whole genome and exome sequencing datasets from five different technologies. When the datasets had discordant genotypes, we arbitrated between them using characteristics of bias typically used for filtering variants, such as strand bias, mapping quality, and clipping of reads. Specifically, at sites with discordant genotypes, we used genotypes from datasets that did not have characteristics of bias. If the reason for the discordant genotypes could not be automatically determined using the characteristics of bias (for example, if datasets with no evidence of bias disagreed), then the variant and surrounding region was excluded from the high-confidence regions. Additionally, we excluded regions if all datasets had evidence of bias or fewer than 5 reads with mapping quality >10. We also excluded regions in which current sequencing technologies are prone to errors (specifically, long homopolymers and tandem repeats, segmental duplications, and putative structural variants). The resulting high-confidence calls and high-confidence regions for this pilot genome, based on DNA from subject NA12878, are rapidly being adopted by clinical and research labs to obtain performance metrics such as sensitivity and false discovery rate for new library preparation and informatics methods [3, 27–32].
One whole genome and one Nextera-based whole exome sequencing dataset from the Illumina HiSeq sequencing platform were used in this work. The coverage of coding regions by the Nextera exome kit was found to be better than other standard exome kits, but worse than newer enhanced exome library preparation methods like ‘augmented exome sequencing’ [33]. This sequencing was performed in 2013 and 2014 by two participating institutions of the Genome in a Bottle Consortium: NIST and the Garvan Institute of Medical Research. The sequencing was done on the candidate NIST Reference Material 8398, a large batch of DNA extracted from the cell line GM12878. The cell line is archived at the Coriell Institute for Medical Research. These measurements represent typical approaches that were broadly used at the time of this study.
Whole genome sequencing of 150 × 150 bp paired end reads was performed on the Illumina HiSeq 2500 with PCR-free v2 chemistry at NIST. These data were from 12 flow cells on the same instrument and 14 replicate libraries prepared from a total of six tubes of candidate NIST RM 8398. The raw data were aligned using BWA MEM v.0.7.5a with default parameters [34]. Reads from each library from each lane were independently realigned using GATK v.2.8-1-g932cd3a IndelRealigner, followed by Base Quality Score Recalibration following GATK Best Practices [35]. Then, all reads from all runs and libraries were combined for a second round of GATK IndelRealigner. The reads were randomly downsampled from approximately 300× to 30× coverage to give a typical level of coverage for WGS. Note that this amounted to 31× coverage within the Nextera exome capture regions. Even though these data are from multiple libraries and runs, we expect that these should represent typical data for the purposes of this work, though they may contain slightly fewer errors since errors from any particular library would be diluted by combining with other libraries. Variants were called using Platypus v.0.5.2 including assembly-based calling to test a new pipeline that was recently proposed for clinical variant calling [36]. Variants were filtered using the defaults for Platypus (that is, GOF, badReads, alleleBias, hp10, Q20, HapScore, MQ, strandBias, SC, QualDepth, REFCALL, and QD) [36]. Separately, INDELs were called using Scalpel [37] version 0.3.2 in single sample mode for CCDS regions with default settings. The entire 300× dataset and the 30× downsampled bam file are available on the GIAB ftp site at NCBI: ftp://ftp-trace.ncbi.nlm.nih.gov/giab/ftp/data/NA12878/NIST_NA12878_HG001_HiSeq_300x/.
Approximately 50× coverage whole exome sequencing was performed on a library prepared using the Nextera rapid capture exome kit at the Garvan Institute of Medical Research. The raw read data were aligned using BWA and variants were called using GATK HaplotypeCaller v.2.7-2-g6bda569 [35]. No filtering was applied. Note that the variant calling pipelines for WES differs from that of the WGS. The vcf file used is available on the GIAB ftp site at NCBI: ftp://ftp-trace.ncbi.nlm.nih.gov/giab/ftp/data/NA12878/analysis/GARVAN_snps_indels_12172013/project.NIST.hc.snps.indels.vcf Separately, INDELs were called using Scalpel [37] version 0.3.2 in single sample mode for CCDS regions with default settings.
Comparison to GIAB benchmark calls
We compared the WGS and WES calls to the latest version of high-confidence calls from GIAB, which integrates multi-platform integrated calls from NIST with two phased pedigree call sets from Real Time Genomics and the Illumina Platinum Genomes Project (from: ftp://ftp-trace.ncbi.nlm.nih.gov/giab/ftp/release/NA12878_HG001/GIABPedigreev0.2/). To compare different representations of complex variants (that is, nearby SNVs and/or indels), we used the freely available Real Time Genomics tool vcfeval (ftp://ftp-trace.ncbi.nlm.nih.gov/giab/ftp/tools/RTG/). The resulting calls in the test sets that were included (true positives), extra (false positives), and missing (false negatives) in the benchmark were then annotated for potential functional effect.
Annotation and variant classification
We annotated variant call sets with Sequence to Medical Phenotypes (STMP), which employs a custom Annovar-based tool to integrate data into a tabular format from 94 sources, including segmental duplications, repetitive elements, ClinVar and OMIM annotations, and performs separate functional annotations with transcript information from NCBI RefSeq, Ensembl, and UCSC [1, 38]. The data were further sorted and variants tabulated with custom python scripts. Individual variants were manually curated for technical validity (JZ) and potential clinical relevance (MG).
Gene sets
We define two gene sets. The American College of Medical Genetics and Genomics (ACMG) reportable genes list contains the 56 genes that the ACMG recommend for pathogenic variant discovery and reporting [39]. Though it contains only a fraction of important disease-related genes, we selected the list because it represents an externally defined minimal set of genes where performance must meet clinical standards. It also represents a group of genes felt to be medically actionable, a group where we would hope for optimal technical performance. The second gene set contains genes derived from the ClinVar and OMIM catalogs to represent a total of 3,300 genes with known relationship to human disease.
Genomic regions
The 35 bp uniqueness scores and 100 bp alignability data were downloaded from the UCSC Genome Browser. The Z bp uniqueness metric indicates whether the sequence (of length-Z) beginning at that base is unique in the genome, while the 100 bp ‘alignability’ metric tolerates up to two mismatches.
The 100 bp uniqueness scores were created by breaking the reference into 100 bp fragments and aligning with Bowtie (allowing no gaps and only accepting unique alignments, options: −v0 –best –m1).
Sites with systematic errors in relevant databases
We defined sites with systematic errors as sites that were first determined to be homozygous reference by the Genome in a Bottle arbitration process, and second, a non-homozygous reference genotype was called from any sequencing platforms that had reads containing a variant at the site. Specifically, we considered a site to have a systematic error if all sequencing datasets from a platform had evidence for an incorrect genotype or if more than two sequencing datasets from a platform had evidence for an incorrect genotype. No filtering was performed and all variants with a quality score >2 were called using GATK v2.8-1. A low quality score threshold was used to be more comprehensive in finding sites that might have bias. These sites can be downloaded from the GIAB ftp site (ftp://ftp-trace.ncbi.nlm.nih.gov/giab/ftp/data/NA12878/analysis/NIST_union_callsets_06172013/NISTIntegratedCalls_14datasets_131103_allcall_UGHapMerge_HomRef_VQSRv2.18_all_bias_nouncert_excludesimplerep_excludesegdups_excludedecoy_excludeRepSeqSTRs_noCNVs.vcf.gz), and the platform or platforms with systematic errors are listed in the INFO field, ‘platformbias’. We used bedtools [40] to intersect the coordinates of these variants with those in annotation databases and custom perl scripts to filter out variants in annotation databases with different alternative alleles.
Characterizing the GIAB high-confidence regions
We restricted benchmarking to regions of the Genome in a Bottle reference material determined to be high confidence. As described above and in our previous work [26], we excluded regions from the high-confidence regions if they were low coverage, prone to mapping error (paralogous sequences, repetitive elements, structural variants, and segmental duplications) or systematic errors in all sequencing chemistries (repetitive elements, low-complexity regions). We characterized the high-confidence regions in terms of uniqueness, repeat sequences, and the proportion of the genome and exome that fall inside these high-confidence regions.
Results
Accuracy of variant calls in high-confidence regions
In the high-confidence regions, we assessed the accuracy of variant calls from Illumina whole genome (BWA MEM followed by Platypus) and Illumina Nextera exome sequencing (BWA followed by GATK).
Sensitivities for whole genome sequencing (WGS) and whole exome sequencing (WES) SNVs
Function | Gene set | WGS SNV sensitivity | WES SNV sensitivity |
|---|---|---|---|
Non-synonymous | ClinVarOMIM | 0.979 (0.970,0.985) | 0.936 (0.923,0.948) |
Non-synonymous | Exome | 0.979 (0.975,0.982) | 0.936 (0.930,0.942) |
Splicing | ClinVarOMIM | 0.889 (0.565,0.994) | 0.556 (0.267,0.811) |
Splicing | Exome | 0.951 (0.865,0.983) | 0.629 (0.505,0.738) |
Synonymous | ClinVarOMIM | 0.988 (0.982,0.992) | 0.952 (0.942,0.961) |
Synonymous | Exome | 0.985 (0.983,0.988) | 0.952 (0.947,0.956) |
Truncating | ClinVarOMIM | 1.000 (0.646,1.000) | 1.000 (0.646,1.000) |
Truncating | Exome | 1.000 (0.924,1.000) | 0.915 (0.801,0.966) |
Whole genome | N/A | 0.954 (0.954,0.955) | 0.053 (0.053,0.053) |
False negatives and false positives arise for different reasons in each platform. For WES, poor read depth was the primary driver of sensitivity as 95 % of false negative variants (FNVs) fell within regions having a read coverage of <10. Note that variant calls remained consistent with increased overall coverage (Additional file 1: Table S1). Further analysis of FNVs revealed that 16 % of whole genome FNVs fall inside simple repeats, low complexity regions, or satellite repeats, compared to 8.6 % of whole exome FNVs. In contrast, 16 % of whole exome FNVs are in regions with GC content >75 %, compared to <1 % of whole genome FNVs.
For WGS, most FNVs resulted from filtering by Platypus due to their presence within difficult-to-sequence and/or difficult-to-call regions. Specifically, 87 % of FNVs were called but removed by filtering using the default parameterization of Platypus (that is, low base qualities, allele frequency, homopolymers >10 bp, variant quality <20, too many haplotypes, low mapping quality, strand bias, low complexity regions). Thirty-six percent of whole genome FNVs fell within the short interspersed nuclear elements (SINE) class of repetitive elements, compared to 13 % of all whole genome bases residing within SINEs, and less than 1 % of FNVs within genic SINEs. Since most FNVs for WGS calls in the whole genome were caused by filtering, we characterized which filters were most and least specific in distinguishing likely false positives from likely true positives (Additional file 2: Table S2). The least specific filters for Platypus were haplotype score (HapScore), mapping quality (MQ), sequence context (SC), and QUAL by depth (QD). When these were the only filters, they contained only 3 % to 5 % false positives and together made up 77 % of the FNVs. In contrast, strandBias, a filter indicating that a significantly higher proportion of variants falls on one sequencing strand compared to the other, contained 68 % false positives when it occurred on its own or 99 % false positives when it occurred in addition to another filter. In general, sites with multiple reasons for filtering had a higher false positive rate (39 %) than all filtered sites (15 %). These results highlight the importance of characterizing and tuning filters to obtain the most accurate and complete call-set possible [41].
Less than 3 % of variants in both whole genome and exome sequencing were absent from benchmark calls but fell within high-confidence regions; therefore, one could consider these variants false positives. However, manual inspection of alignments around these variants suggests a variety of etiologies, so we instead call them questionable variants (QVs). For WES, most QVs were correctly identified as non-reference but had incorrect genotypes due to insufficient coverage (for example, the sites were identified as homozygous variant when they were in fact heterozygous). Since exome variant calls were unfiltered, there were also a few QVs that were likely to be systematic sequencing errors; these had clear evidence of strand bias and would be easily filtered if a strand bias filter were applied, including a variant rs200691513 (K856N) in the clinically-relevant, ACMG gene DSG2, which is associated with arrhythmogenic right ventricular cardiomyopathy. For WGS, almost all of the QVs represent difficulties in our simple classification schema, in that many likely represent true variants occurring near the boundary between high-confidence and low-confidence regions. In fact, except for a series of seven QVs in SERPINA1 (discussed below), all six of the remaining synonymous and non-synonymous QVs in ClinVar/OMIM genes were within 50 bp of the inside edge of high-confidence regions. Complex variants are occasionally missing from the high-confidence calls as they overlap the borders of the high and low confidence delineation. Therefore, we recommend manual inspection of QVs near the edge of high-confidence regions.
In one particular region, appropriate alignments and variant calls against the hg19 reference yielded a series of five synonymous and two non-synonymous phased heterozygous QVs between chr14:94844936-94844975 in the gene, SERPINA1 (Additional file 3: Figure S1a). As shown in Additional file 3: Figure S1b, this gene resides within a larger region that has a curation issue from the Genome Reference Consortium (GRC Curation Issue HG-1930, http://www.ncbi.nlm.nih.gov/projects/genome/assembly/grc/human/issues/?id=HG-1930). These variants are contained in a new alternative sequence that is part of GRCh38 constructed from the 1000 Genomes decoy reference sequence. The GeT-RM browser allows a BLAST search of the sequence in a region, revealing the same series of SNVs in the homologous sequence (Additional file 3: Figure S1c). These seven variants were classified as QVs, because they come from an alternate locus that is unlocalized in the reference assembly. This result highlights that future work is needed to further understand how alternate loci in GRCh38 will be employed in variant calling pipelines to minimize the types of errors classified as QVs and FNVs in our analysis.
Sites prone to systematic errors may have clinical relevance
Sites with falsely-called variants in one or more technologies and their presence in several databases
Sites (n) | |
|---|---|
Total variants with bias | 39,301 |
Total variants with bias in databases | 7,467 |
ClinVar | 4 |
ESP | 38 |
1000 Genomes | 89 |
dbSNP (v138) | 7,363 |
COSMIC | 123 |
Large areas of medically actionable genes fall within low confidence regions
a The fraction of each ACMG gene within GIAB high-confidence regions. b Violin plots showing the distribution of the fraction each gene in the GIAB high-confidence regions for NA12878 for relevant gene sets: ACMG reportable genes, genes with variants in OMIM or ClinVar, and all genes. c Boxplots showing the distribution of the fraction of first, second, middle, penultimate, and last exon in ClinVar or OMIM genes in the GIAB high-confidence regions
Reasons for low confident bases in ACMG genes
Reason for low confidence | Percentage of bases |
|---|---|
CNVs or other SVs that have been reported in dbVar for NA12878 | 47 |
STRs in RepSeqSTRdb | 34 |
Regions with known segmental duplications | 15 |
Simple Repeats from repeat masker | 1.7 |
<3 datasets have at least 5 reads with mapping quality >10 | 1.3 |
Abnormal allele balance | 0.17 |
Unresolved conflicting genotypes after arbitration | 0.03 |
Calls with support from <3 datasets after arbitration | 0.0082 |
Local alignment problems | 0.0041 |
Next, we calculated the proportion of exonic bases present in the high-confidence regions for ClinVar and OMIM genes and all coding genes (Fig. 2b). Surprisingly, only 74.6 % of ClinVar and OMIM genes’ exonic bases and 72.7 % of the exonic bases in all coding genes are found in high-confidence regions. Of the 18,667 coding genes, 990 were 100 % within high-confidence regions; these genes tend to be smaller (mean: 1,787 bp) than the rest (mean: 3,371 bp).
Large portions of clinically important genes fall outside of the high-confidence regions. A total of 593 of 3,300 ClinVar and OMIM genes have less than 50 % of the exonic bases in high-confidence regions and 2,616 of 18,667 coding genes’ exonic bases are entirely excluded from high-confidence regions.
We also examined ClinVar and OMIM genes at the exon-level; Fig. 2c shows the distribution of the proportion of first, second, middle, penultimate, and last exons inside the high-confidence regions. Notably, first exons have a lower than average proportion of their bases in high-confidence regions, which is likely explained by the well-known higher GC content in first exons.
High-confidence regions are enriched for unique and non-repetitive sequences
a The number of sites in the genome where each 35 bp sequence appears for Genome in a Bottle high-confidence and low-confidence regions. b The fraction of each RepeatMasker repeat class in high-confidence regions
Characterizing ClinVar pathogenic variants
Genomic context of ClinVar (likely) pathogenic SNVs
n | % | |
|---|---|---|
Total likely pathogenic or pathogenic SNVs | 15,735 | |
Likely pathogenic or pathogenic SNVs in high-confidence regions | 12,138 | 77.14 |
Likely pathogenic or pathogenic SNVs that start a 35 bp unique sequencea | 15,289 | 97.17 |
Likely pathogenic or pathogenic SNVs that start a 100 bp alignable sequenceb | 15,438 | 98.11 |
Total likely pathogenic or pathogenic SNVs with > = level 2 ClinVar review status [32] | 1,212 | |
Likely pathogenic or pathogenic SNVs with > = level 2 ClinVar review status in high-confidence regions | 998 | 82.34 |
Likely pathogenic or pathogenic SNVs with > = level 2 ClinVar review status that start a 35 bp unique sequencea | 1,190 | 98.18 |
Likely pathogenic or pathogenic SNVs with > = level 2 ClinVar review status that start a 100 bp alignable sequenceb | 1,195 | 98.60 |
Bar graphs displaying the fraction of ClinVar pathogenic or likely pathogenic SNVs in high-confidence regions, unique sequences (35 bp), and alignable sequences (100 bp). The black line represents the genome-wide value
ClinVar variants within ACMG genes in the ExAC database. Depth of coverage in log2 space versus the number of samples that were unable to be called for that variant. The size of the points is relative to quality scores from GATK during joint calling. Orange indicates that the variant is in a high-confidence NA12878 region while blue is considered to be in low confidence. Triangles highlight variants that failed VQSR filtering
Discussion
To better understand the clinical impact of technical aspects of genome sequencing, we used high-confidence consensus calls from a benchmark genome to characterize clinically relevant genetic variation at the gene and variant level across the genome. We characterized the high-confidence regions and examined the proportion of medically relevant genes that fall outside of high-confidence regions.
Disease causing variation occurs in complex regions of the genome
We report that large areas of key genes, as well as a significant proportion of known disease-causing variation, lie outside of high-confidence regions, highlighting the importance of technical accuracy in benchmarking clinical genomics. While less than 1,000 genes across the genome are found entirely within the high-confidence regions, it is perhaps more concerning that, of the genes we regard as most medically important – the ‘actionable’ list of 56 genes from the ACMG, only 82.1 % of their exonic structure is found within high-confidence regions. Indeed, the knowledge that nearly one fifth of each gene, for which laboratory directors are recommended to provide clinical reporting for every patient undergoing clinical exome or genome sequencing, would not reach consensus across different chemistries and pipelines, is sobering. But it is a call to arms for those interested in clinical grade technical accuracy for genome sequencing. We hope by highlighting and scrutinizing the challenging areas of the genome, we can optimize our pipelines for greater consensus and, at the very least, provide transparency regarding our confidence level in every call. In contrast with the lack of immediate personal implication of a false call in a discovery cohort study, a false call on a clinical report could have immediate detrimental consequences in the life of an individual, family, or disease community.
False negative and false positive variants may have clinical impact
Our analysis revealed false negatives and false positives in both WES and WGS. For exome sequencing, many of false negatives were due to low or no coverage, which emphasizes the importance of choosing a sequencing platform that adequately covers all medically-relevant genomic regions [33]. Most false negatives from WGS resulted from overly aggressive filtering.
In one example of a false positive from our systematic error call set, one sequencing chemistry and one pipeline called a recognized, pathogenic frameshift deletion in BRCA2. Pathogenic variants in the BRCA genes are implicated in hereditary breast and ovarian cancer syndrome (http://www.ncbi.nlm.nih.gov/books/NBK1247/). The variant, rs80359760, is currently categorized in ClinVar as pathogenic/likely pathogenic based on several entries from the Breast Cancer Information Core, the Sharing Clinical Reports Project, and the literature (http://www.ncbi.nlm.nih.gov/clinvar/variation/52831/). Based on GIAB’s consensus sequence, this variant is known to be a false positive call for this patient. However, it might be reported to another patient as an incidental finding, and one with evidence for pathogenicity that might even lead to medical action. Examples like this highlight the importance of confirmatory testing by an orthogonal method. Additionally, we hope that our analyses and the reference materials can provide helpful meta-data for bioinformatics analysis of loci such as these, since this dataset allows positions with systematic biases and medically relevant annotations in public databases to be identified [44, 45].
Analytical choices impact variant calls
Our findings highlight the influence of informatic choices upon the final variant calls. For example, the newest human reference GRCh38 employs alternate contigs, encompassing a more accurate but complex representation of normal human variation. To maximize the benefit from this significant advance requires the development of mapping, variant calling, and variant comparison [46] software that recognizes complex variation (for example, SERPINA1 variation corresponding to an alternate locus in GRCh38, see Results) [47]. Additionally, the choice of ethnicity-specific reference genomes has been shown to impact the sensitivity of variant calling [19]. Furthermore, differences within the annotation schema employed may also influence the clinical impact of the call set [48]. Within the ACMG 56 genes in the NA12878 true positive confident call set, there were five variants that were annotated differently by one of the three gene models employed (see Additional file 6: Table S5). For example, the voltage-gated sodium channel, SCN5A, is associated with dilated cardiomyopathy and long QT syndromes and displays a complex developmentally-regulated pattern of multiple splice isoforms [49]. Though the common variant rs6599230 is unlikely to be of functional significance, it was annotated as a synonymous variant p.A29A using Refgene and Gencode transcript models, and alternately annotated as a non-synonymous variant p.Q32R with a UCSC Knowngene transcript model. Each of these annotations is a true and accurate representation, each corresponding to a different splice isoform and supported by either computationally-predicted or manually-curated transcript data. However, among the multiplicity of variants, it is not clear which (or all) of these should be displayed to the ordering clinician for the purposes of clinical decision-making. Disease domain specific expertise and standardization efforts, such as those already in process by the ClinGen Resource (http://clinicalgenome.org/) will prove necessary to develop the most clinically appropriate gene models or transcripts for a particular gene. Additionally, emerging resources such as the Genotype-Tissue Expression (GTEx) project may provide relevant information for deconvoluting the isoform specific mutations in the tissue of interest.
Conclusions
Using the reference materials developed by the Genome in a Bottle Consortium, we show that the predictive characteristics of WES and WGS for any given variant appear to depend on the genomic region, the class of variant, and the informatic tools employed. We discuss false positive and questionable variant calls from these reference materials that could significantly impact clinical care. Thus, the discussion of the technical aspects of clinical sequencing, and the continued development of reference materials to characterize more challenging parts of the genome, are critical steps toward enabling a better understanding of the predictive and technical characteristics of these tests.
Declarations
Acknowledgments
We thank Jiang Tao and colleagues at the Garvan Institute of Medical Research for contributing the exome sequencing data used in this work to the Genome in a Bottle Consortium. Certain commercial equipment, instruments, or materials are identified in this report to specify adequately the experimental procedure. Such identification does not imply recommendation or endorsement by the National Institute of Standards and Technology, nor does it imply that the materials or equipment identified are necessarily the best available for the purpose. JRP is supported by the Pediatric Scientist Development Program, (NIH-NICHD K12-HD000850). RLG is supported by the National Library of Medicine Training Grant T15 LM7033 and an NSF graduate research fellowship. MEG's current address is Stanford Health Care, Stanford, California. The information presented represents the author’s own views and does not necessarily represent the views of Stanford Hospital and Clinics, Lucile Packard Children’s Hospital and/or Stanford University or its affiliates.
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Authors’ Affiliations
References
- Dewey FE, Grove ME, Pan CP, Goldstein BA, Bernstein JA, Chaib H, et al. Clinical Interpretation and Implications of Whole-Genome Sequencing. JAMA. 2014;311:1035–44.PubMed CentralView ArticlePubMedGoogle Scholar
- Dewey FE, Grove ME, Priest JR, Waggott D, Batra P, Miller CL, et al. Sequence to Medical Phenotypes: A Framework for Interpretation of Human Whole Genome DNA Sequence Data. PLoS Genet. Public Library of Science. 2015;11(10):e1005496. Google Scholar
- Meynert AM, Ansari M, FitzPatrick DR, Taylor MS. Variant detection sensitivity and biases in whole genome and exome sequencing. BMC Bioinformatics. 2014;15:247.PubMed CentralView ArticlePubMedGoogle Scholar
- Fang H, Wu YY, Narzisi G, O’Rawe JA, Barron LTJ, Rosenbaum J, et al. Reducing INDEL calling errors in whole genome and exome sequencing data. Genome Med. 2014;6:17.View ArticleGoogle Scholar
- O’Rawe J, Jiang T, Sun GQ, Wu YY, Wang W, Hu JC, et al. Low concordance of multiple variant-calling pipelines: practical implications for exome and genome sequencing. Genome Med. 2013;5:18.View ArticleGoogle Scholar
- Wall JD, Tang LF, Zerbe B, Kvale MN, Kwok PY, Schaefer C, et al. Estimating genotype error rates from high-coverage next-generation sequence data. Genome Res. 2014;24:1734–9.PubMed CentralView ArticlePubMedGoogle Scholar
- Meienberg J, Zerjavic K, Keller I, Okoniewski M, Patrignani A, Ludin K, et al. New insights into the performance of human whole-exome capture platforms. Nucleic Acids Res. 2015;43:e76.PubMed CentralView ArticlePubMedGoogle Scholar
- Parla JS, Iossifov I, Grabill I, Spector MS, Kramer M, McCombie WR. A comparative analysis of exome capture. Genome Biol. 2011;12:R97.PubMed CentralView ArticlePubMedGoogle Scholar
- Clark MJ, Chen R, Lam HYK, Karczewski KJ, Euskirchen G, Butte AJ, et al. Performance comparison of exome DNA sequencing technologies. Nat Biotechnol. 2011;29:908–14.PubMed CentralView ArticlePubMedGoogle Scholar
- de Koning AP, Gu W, Castoe TA, Batzer MA, Pollock DD. Repetitive elements may comprise over two-thirds of the human genome. PLoS Genet. 2011;7:e1002384.PubMed CentralView ArticlePubMedGoogle Scholar
- Clamp M, Fry B, Kamal M, Xie X, Cuff J, Lin MF, et al. Distinguishing protein-coding and noncoding genes in the human genome. Proc Natl Acad Sci U S A. 2007;104:19428–33.PubMed CentralView ArticlePubMedGoogle Scholar
- Moreau A, Gosselin-Badaroudine P, Chahine M. Biophysics, pathophysiology, and pharmacology of ion channel gating pores. Front Pharmacol. 2014;5:53.PubMed CentralView ArticlePubMedGoogle Scholar
- MacArthur DG, Balasubramanian S, Frankish A, Huang N, Morris J, Walter K, et al. A systematic survey of loss-of-function variants in human protein-coding genes. Science. 2012;335:823–8.PubMed CentralView ArticlePubMedGoogle Scholar
- Choi M, Scholl UI, Ji W, Liu T, Tikhonova IR, Zumbo P, et al. Genetic diagnosis by whole exome capture and massively parallel DNA sequencing. Proc Natl Acad Sci U S A. 2009;106:19096–101.PubMed CentralView ArticlePubMedGoogle Scholar
- Gonzaga-Jauregui C, Lupski JR, Gibbs RA. Human genome sequencing in health and disease. Annu Rev Med. 2012;63:35–61.PubMed CentralView ArticlePubMedGoogle Scholar
- Ley TJ, Mardis ER, Ding L, Fulton B, McLellan MD, Chen K, et al. DNA sequencing of a cytogenetically normal acute myeloid leukaemia genome. Nature. 2008;456:66–72.PubMed CentralView ArticlePubMedGoogle Scholar
- Link DC, Schuettpelz LG, Shen D, Wang J, Walter MJ, Kulkarni S, et al. Identification of a novel TP53 cancer susceptibility mutation through whole-genome sequencing of a patient with therapy-related AML. JAMA. 2011;305:1568–76.PubMed CentralView ArticlePubMedGoogle Scholar
- Ashley EA, Butte AJ, Wheeler MT, Chen R, Klein TE, Dewey FE, et al. Clinical assessment incorporating a personal genome. Lancet. 2010;375:1525–35.PubMed CentralView ArticlePubMedGoogle Scholar
- Dewey FE, Chen R, Cordero SP, Ormond KE, Caleshu C, Karczewski KJ, et al. Phased whole-genome genetic risk in a family quartet using a major allele reference sequence. PLoS Genet. 2011;7:e1002280.PubMed CentralView ArticlePubMedGoogle Scholar
- Priest JR, Ceresnak SR, Dewey FE, Malloy-Walton LE, Dunn K, Grove ME, et al. Molecular diagnosis of long QT syndrome at 10 days of life by rapid whole genome sequencing. Heart Rhythm. 2014;11:1707–13.PubMed CentralView ArticlePubMedGoogle Scholar
- Willig LK, Petrikin JE, Smith LD, Saunders CJ, Thiffault I, Miller NA, et al. Whole-genome sequencing for identification of Mendelian disorders in critically ill infants: a retrospective analysis of diagnostic and clinical findings. Lancet Respir Med. 2015;3:377–87.View ArticlePubMedGoogle Scholar
- Soden SE, Saunders CJ, Willig LK, Farrow EG, Smith LD, Petrikin JE, et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci Transl Med. 2014;6:265ra168.PubMed CentralView ArticlePubMedGoogle Scholar
- Saunders CJ, Miller NA, Soden SE, Dinwiddie DL, Noll A, Abu Alnadi N, et al. Rapid whole-genome sequencing for genetic disease diagnosis in neonatal intensive care units. Sci Transl Med. 2012;4:154ra135.PubMed CentralView ArticlePubMedGoogle Scholar
- Kingsmore SF, Petrikin J, Willig LK, Guest E. Emergency medical genomes: a breakthrough application of precision medicine. Genome Med. 2015;7:82.PubMed CentralView ArticlePubMedGoogle Scholar
- Highnam G, Wang JJ, Kusler D, Zook J, Vijayan V, Leibovich N, et al. An analytical framework for optimizing variant discovery from personal genomes. Nat Commun. 2015;6:6.View ArticleGoogle Scholar
- Zook JM, Chapman B, Wang J, Mittelman D, Hofmann O, Hide W, et al. Integrating human sequence data sets provides a resource of benchmark SNP and indel genotype calls. Nat Biotechnol. 2014;32:246–51.View ArticlePubMedGoogle Scholar
- Aziz N, Lynn B, Driscoll D, Gibson J, Grody W, Hegde M, et al. College of American pathologists’ laboratory standards for next generation sequence clinical testing. J Mol Diagn. 2012;14:742.Google Scholar
- Cantarel BL, Weaver D, McNeill N, Zhang JH, Mackey AJ, Reese J. BAYSIC: a Bayesian method for combining sets of genome variants with improved specificity and sensitivity. BMC Bioinformatics. 2014;15:104.PubMed CentralView ArticlePubMedGoogle Scholar
- Cleary JG, Braithwaite R, Gaastra K, Hilbush BS, Inglis S, Irvine SA, et al. Joint variant and de novo mutation identification on pedigrees from high-throughput sequencing data. J Comput Biol. 2014;21:405–19.View ArticlePubMedGoogle Scholar
- Klein HG, Bauer P, Hambuch T. Whole genome sequencing (WGS), whole exome sequencing (WES) and clinical exome sequencing (CES) in patient care. LaboratoriumsMedizin-Journal of Laboratory Medicine. 2014;38:221–30.Google Scholar
- Xu HL, DiCarlo J, Satya RV, Peng Q, Wang YX. Comparison of somatic mutation calling methods in amplicon and whole exome sequence data. BMC Genomics. 2014;15:244.PubMed CentralView ArticlePubMedGoogle Scholar
- Linderman MD, Brandt T, Edelmann L, Jabado O, Kasai Y, Kornreich R, et al. Analytical validation of whole exome and whole genome sequencing for clinical applications. BMC Med Genomics. 2014;7:20.PubMed CentralView ArticlePubMedGoogle Scholar
- Patwardhan A, Harris J, Leng N, Bartha G, Church DM, Luo S, et al. Achieving high-sensitivity for clinical applications using augmented exome sequencing. Genome Med. 2015;7:71.PubMed CentralView ArticlePubMedGoogle Scholar
- Li H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. arXiv:13033997 [q-bioGN] 2013.Google Scholar
- DePristo MA, Banks E, Poplin R, Garimella KV, Maguire JR, Hartl C, et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nature Genetics. 2011;43:491–8.PubMed CentralView ArticlePubMedGoogle Scholar
- Rimmer A, Phan H, Mathieson I, Iqbal Z, Twigg SRF, Wilkie AOM, et al. Integrating mapping-, assembly- and haplotype-based approaches for calling variants in clinical sequencing applications. Nat Genet. 2014;46:912–8.PubMed CentralView ArticlePubMedGoogle Scholar
- Narzisi G, O'Rawe JA, Iossifov I, Fang H, Lee YH, Wang ZH, et al. Accurate de novo and transmitted indel detection in exome-capture data using microassembly. Nat Methods. 2014;11:1033–6.PubMed CentralView ArticlePubMedGoogle Scholar
- Wang K, Li MY, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38:e164.PubMed CentralView ArticlePubMedGoogle Scholar
- Green RC, Berg JS, Grody WW, Kalia SS, Korf BR, Martin CL, et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet Med. 2013;15:565–74.PubMed CentralView ArticlePubMedGoogle Scholar
- Quinlan AR, Hall IM. BEDTools: a flexible suite of utilities for comparing genomic features. Bioinformatics. 2010;26:841–2.PubMed CentralView ArticlePubMedGoogle Scholar
- Gargis AS, Kalman L, Bick DP, da Silva C, Dimmock DP, Funke BH, et al. Good laboratory practice for clinical next-generation sequencing informatics pipelines. Nat Biotechnol. 2015;33:689–93.View ArticlePubMedGoogle Scholar
- She XW, Jiang ZX, Clark RL, Liu G, Cheng Z, Tuzun E, et al. Shotgun sequence assembly and recent segmental duplications within the human genome. Nature. 2004;431:927–30.View ArticlePubMedGoogle Scholar
- Lek M, Karczewski K, Minikel E, Samocha K, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. BioRxiv. 2015. doi: 10.1101/030338.
- Alkan C, Sajjadian S, Eichler EE. Limitations of next-generation genome sequence assembly. Nat Methods. 2011;8:61–5.PubMed CentralView ArticlePubMedGoogle Scholar
- Chaisson MJ, Huddleston J, Dennis MY, Sudmant PH, Malig M, Hormozdiari F, et al. Resolving the complexity of the human genome using single-molecule sequencing. Nature. 2015;517:608–11.PubMed CentralView ArticlePubMedGoogle Scholar
- Cleary JG, Braithwaite R, Gaastra K, Hilbush BS, Inglis S, Irvine SA, et al. Comparing variant call files for performance benchmarking of next-generation sequencing variant calling pipelines. 2015. doi: 10.1101/023754.
- Rosenbloom KR, Armstrong J, Barber GP, Casper J, Clawson H, Diekhans M, et al. The UCSC Genome Browser database: 2015 update. Nucleic Acids Res. 2015;43(Database Issue):D670–81.PubMed CentralView ArticlePubMedGoogle Scholar
- McCarthy DJ, Humburg P, Kanapin A, Rivas MA, Gaulton K, Cazier JB, et al. Choice of transcripts and software has a large effect on variant annotation. Genome Med. 2014;6:26.PubMed CentralView ArticlePubMedGoogle Scholar
- van Stuijvenberg L, Yildirim C, Kok BG, van Veen TA, Varró A, Winckels SK, et al. Alternative promoter usage and splicing of the human SCN5A gene contribute to transcript heterogeneity. DNA Cell Biol. 2010;29:577–87.View ArticlePubMedGoogle Scholar